CHRONIC PANCREATITIS
67 year old male with Pain Abdomen
13/12/22
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
K.Medha Reddy, intern
Roll No: 61
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE:
A 67 year old male, resident of kodhada, farmer by occupation, came to the hospital with chief complaints of:
Pain Abdomen since 3 months.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently assymptomatic 3 months ago, then he developed pain abdomen, which is continuous, insidious in onset, gradually progressive, squeezing type, non radiating, aggravated on coughing and deep inspiration and relieved on lying down down on right side.
H/O loss of weight from the past 3 months (10kgs)
No H/O vomitings or gurgitation
No H/O malena
No H/O hematemesis
No H/O nausea
No H/O cough
No H/O fever
PAST HISTORY:
Pt is Not a K/C/O DM / HTN / TB / Asthma / Epilepsy / CVA / CAD
H/O NSAID use on and off from past one year, but continuously from the past 3 months.
No previous surgical history
No drug or food allergy
No previous history of TB
PERSONAL HISTORY:
Appetite: Decreased due to pain
Diet: Mixed
Sleep: adequate
Bowel and bladder: regular
Addictions:
History of Alcohol consumption since 47 years. last intake was 3 months ago.
History of smoking from at the age of 14 years, slowly increased to consuming 2packs (50) cigarettes per day for the past 53 years. Stopped smoking frequently from the past 3 months.
FAMILY HISTORY:
No significant family history
No History of TB in the family
GENERAL EXAMINATION:
Patient is conscious, cohorent, cooperative and well oriented to time, place and person.
Pallor- present
Icterus- absent
Clubbing-absent
Lymphadenopathy- absent
Cyanosis- absent
Pedal edema - absent
VITALS: on 12.12.2022
B.P: 110/70 mmhg
P.R: 85bpm
R.R: 16 cpm
Temp: 98.3 F
SPO2: 98% on RA
GRBS: 405mg/dl
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection:
Drooping of shoulder + towards right side.
No tracheal deviation
Chest bilaterally symmetrical
Moving equally with respiration on both sides
No dilated veins,pulsations,scars, sinuses.
Palpation:
No tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Vocal fremitus- normal on both sides (equal)
Anteroposterior diameter- 17.7 cm
Transverse diameter- 25.4 cm
Percussion:
Equally resonant on both sides
(Examined areas - Supra clavicular ,Infra clavicular, Mammary, Axillary, Infra axillary, Supra scapular, Infra scapular, Inter scapular)
Auscultation: Right Left
Supra clavicular: NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Axillary: NVBS NVBS
Infra axillary: NVBS NVBS
Supra scapular: NVBS NVBS
Infra scapular: NVBS NVBS
Inter scapular: NVBS NVBS
CARDIOVASCULAR SYSTEM:
Inspection:
Shape of chest- normal
JVP - not raised
Palpation:
Apical impulse was felt at 5th intercoastal space 1 cm medial to mid clavicular line
On auscultation :
S1 S2 heard No murmurs .
PER ABDOMEN :
On inspection:
Umbilicus - inverted
All quadrants moving equally with respiration
A blackish patch is seen on the lower abdomen at the umbilical region.
On palpation:
Abdomen is soft
Tenderness present in the right hypogastruim and right lumbar regions
No palpable spleen and liver
Normal bowel sounds heard.
CENTRAL NERVOUS SYSTEM:
All higher mental functions, motor system, sensory system and cranial nerves- intact.
RT LFT
BICEPS 1+. 1+
TRICEPS 1+. 1+
SUPINATOR 1+ 1+
ANKLE 1+. 1+
KNEE 1+. 1+
INVESTIGATIONS:
ECG:
LABS: (All samples)
HB: 8.3 > 9.1 > 8.3 > 7.5 > 7.7 > 8.1
TLC: 18,600 > 21,000 > 32,300 > 14,500 > 16,200 > 18,300
PLT: 4.50 > 5.38 > 6.3 > 4.21 > 3.74 > 4.42
TB: 0.61 > 0.63 > 0.77 > 0.66
DB: 0.16 > 0.27 > 0.20 > 0.20
SGOT: 15 > 17 >17 > 22
SGOT: 27 > 34 > 22 > 37
ALP: 314 > 338 > 255 > 234
TP: 8.0 > 8.6 > 7.5 > 5.9
ALB: 3.0 > 4.5 > 2.8 > 3.1
A/G RATIO: O.61 > 1.2 > 0.62 > 1.09
SERUM AMYLASE : 143 > 133 > 92
SERUM LIPASE : 48 > 26.5 > 29
SERUM UREA: 88 > 83 > 74 > 52 > 65
UA: 7.6 > 6.0
SERUM CREAT: 1.8 > 1.7 > 1.5 > 1.5 > 1.8
Na+ : 132 > 136 > 135 > 135 > 133
K+ : 5.8 > 4.0 > 5.2 > 5.7 > 4.6
Cl- : 103 > 100 > 104 > 105 > 103
Ca+2 : 9.5 > 9.7
PO4- : 4.2
LDH: 220
Serology: Negative
RBS: 405
FBS: 70
HbA1c : 7.2
Serum iron : 66.5
Serum ferritin :
ABG:
CUE:
ALBUMIN : ++
SUGARS: ++++
URINE FOR KETONE BODIES: NEGATIVE
SPOT URINE PROTEIN : 22.1
SPOT URI CREAT : 26.9
RATIO : 0.82
URINARY CHLORIDE: 106
SPOT URINARY POTTASIUM: 5.4
SPOT URINE SODIUM: 62
X RAY REPORTING:
REPEAT XRAY:
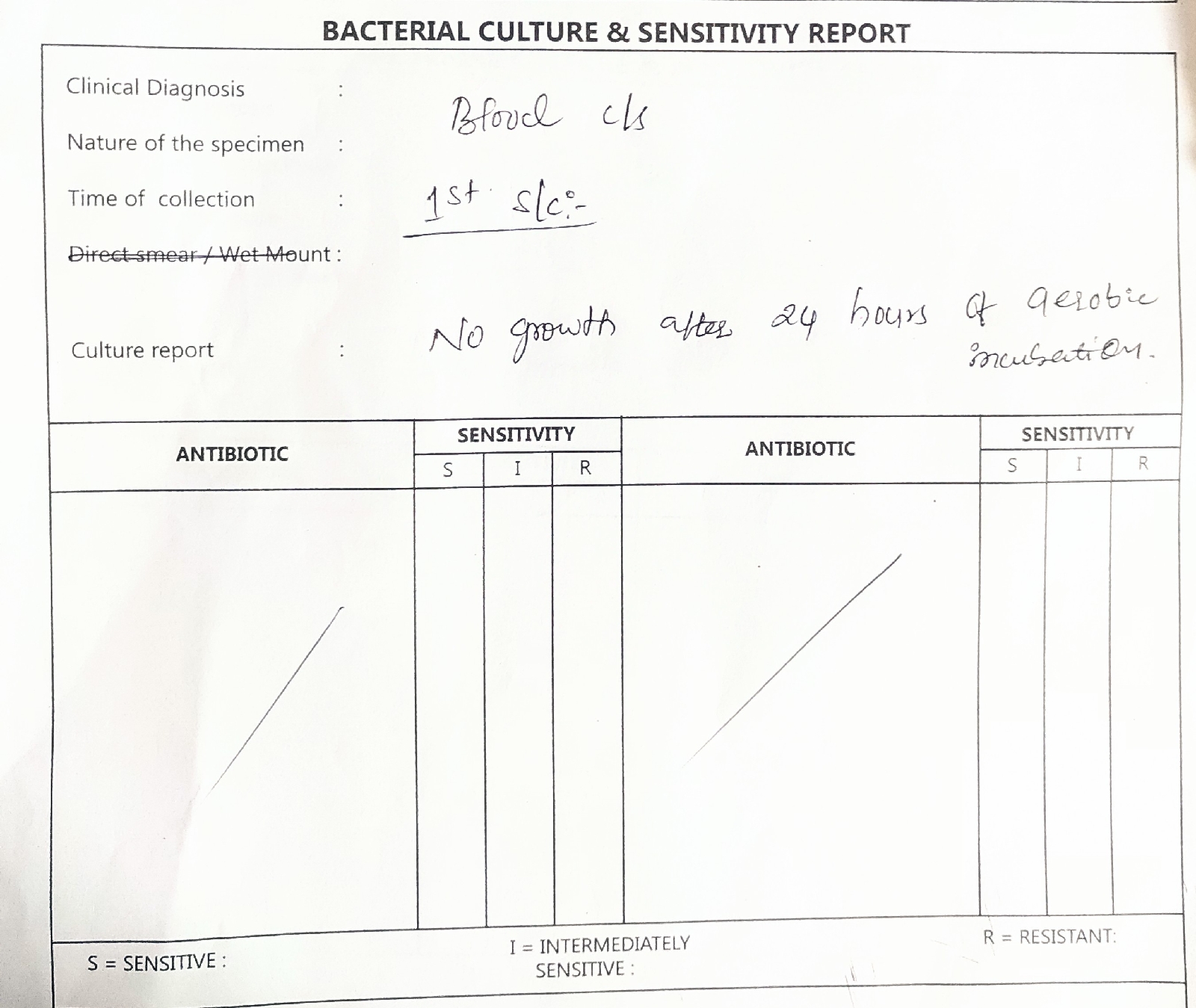
BLOOD C/S:
URINE C/S:
SPUTUM C/S :
PULMONOLOGY OPINION: FOR RENAL DOSE MODIFICATION OF ATT
DIAGNOSIS:
Chronic pancreatitis
TB
?Chronic Pancreatitis causing Diabetes
?AKI due to NSAID Abuse since 3months.
?Acute exacerbation of chronic pancreatitis
TREATMENT:
Date of admission: 12/12/22 at 4:30 pm
Day1: 13/12/22
ICU bed 5:
Patient came with a C/O:
Pain abdomen since 3 months
S: Patient is c/c/c
No new complaints
O: O/E: pt is c/c/c
Afebrile
BP: 100/70 mmHg
PR: 65
Sats: 99
CVS: S1, S2 +
RS: BAE+
P/A: soft, Tenderness + in right hypogastruim and right lumbar region
A: chronic pancreatitis
Chronic pancreatitis causing diabetes ?
? borderline TB
P:
IVF - RL,NS @100mllhr
Inj. MONOCEF 1gm IV BD
Inj. PANTOP 40 mg IV OD
Inj. ZOFER 4mg IV SOS
Inj. TRAMADOL 100mg in 100ml NS IV OD
Inj. HAI 4 units SC TID (Premeal)
Nebulisation with SALBUTAMOL 2 respules
DAY 2: 14/12/22:
AMC : Bed1
S: Patient is c/c/c
No new complaints
O: O/E: pt is c/c/c
Afebrile
BP: 110/60 mmHg
PR: 71 bpm
Sats: 98%
CVS: S1, S2 +
RS: BAE+
P/A: soft, Tenderness + in right hypochondrium and umbilical region
A: chronic pancreatitis
Chronic pancreatitis causing diabetes ?
? TB
P:
IVF - RL,NS @75mllhr
Inj. MONOCEF 1gm IV BD
Inj. PANTOP 40 mg IV OD
Inj. ZOFER 4mg IV SOS
Inj. TRAMADOL 100mg in 100ml NS IV OD
Inj. HAI 4 units SC TID (Premeal)
Nebulisation with SALBUTAMOL 2 respules STAT
DAY 3: 15/12/22
Ward
Patient came with a C/O:
Pain abdomen since 3 months
S: Patient is c/c/c
No new complaints
O: O/E: pt is c/c/c
Afebrile
BP: 120/70 mmHg
PR: 82 bpm
Sats: 98%
CVS: S1, S2 +
RS: BAE+
P/A: soft, Tenderness + in right hypochondrium and right lumbar region
A: chronic pancreatitis
TB
Chronic pancreatitis causing diabetes ?
P:
IVF - 1RL @50ML/HR
Inj. PANTOP 40 mg IV OD
Inj. ZOFER 4mg IV SOS
Inj. TRAMADOL 100mg in 100ml NS IV OD
Inj. HAI 4 units SC TID (Premeal)
Nebulisation with SALBUTAMOL 2 respules
DAY 4 : 16/12/22
WARD
Patient came with a C/O:
Pain abdomen since 3 months. The pain decreased now
He turned out to be AFB and CBNAAT positive (Rifampicin sensitive). He doesn't have any classic TB symptoms like fever and cough. Started him on ATT therapy, HRZE regimen (3pills/day)
S: Patient is c/c/c
No new complaints, stools not passed
O: O/E: pt is c/c/c
Afebrile
BP: 100/70 mmHg
PR: 90 bpm
Sats: 98%
CVS: S1, S2 +, no added heart sounds, no murmurs
RS: BAE+, NVBS
CREPTS + RIGHT ICA.
P/A: soft, Tenderness + in right hypochondrium and umbilical region
A: chronic pancreatitis
TB
?Chronic pancreatitis causing diabetes
P:
IVF - 1RL @50ML/HR
Inj. PANTOP 40 mg IV OD
Inj. ZOFER 4mg IV SOS
Inj. TRAMADOL 100mg in 100ml NS IV OD
Tab. BENADON 40MG PO OD
TAB. OFLOXACIN 200mg PO OD
Inj. HAI 4 units SC TID (Premeal)
Nebulisation with SALBUTAMOL 2 respules
Dermat drugs:
LULIFIN CREAM FOR L/A BD
LIQUID PARAFFIN FOR L/A BD
TAB. DAZIT 5MG PO OD
ATT DRUGS:
ISONIAZID 5mg/kg/bodywt OD
RIFAMPICIN 10mg/kg/bodywt OD
PYRAZINAMIDE 25-35mg/kg/bodywt Thrice weekly
ETHAMBUTOL 15-25mg/kg/bodywt Thrice weekly





















Comments
Post a Comment